Continuous Renal Replacement Therapy (CRRT)
The continuum of kidney dysfunction
Acute Kidney Injury (AKI) is a heterogeneous syndrome1,2 associated with poor patient outcomes with each patient having a unique risk profile and trajectory of disease progression.3,4 The term AKI describes a spectrum of acute kidney dysfunction, as part of the continuum of kidney dysfunction from AKI to Acute Kidney Diseases and Disorders (AKD) to Chronic Kidney Disease (CKD).1,5 Persistent severe AKI can be defined as Stage 3 AKI lasting for ≥ 72 hours and may progress to AKD or CKD.5,6
CRRT is the preferred modality among many clinicians to achieve specific clinical goals for AKI management, providing flexibility to meet the evolving needs of each patient.
AKI associated with poor patient outcomes

Reported incidences vary
The reported incidence of AKI among ICU patients varies from 0.5% to
78.7%7 - 9; up to ~25% of these patients may require RRT.12 - 15

Risk of mortality
AKI is associated with an increased risk of morbidity16 - 26 and short- and long-term mortality.27 - 30

Progression to CKD
AKI is associated with an increased risk of progression to CKD, including ESRD.28,31
A cornerstone treatment for patients with severe AKI32
Renal Replacement Therapy (RRT) represents a major component of AKI management, particularly in severe cases, with different modalities to address the patient’s evolving clinical needs during the course of disease.
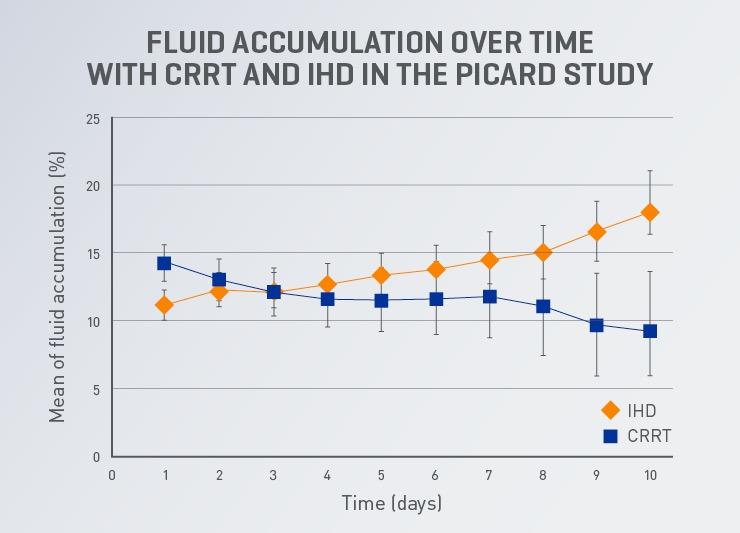
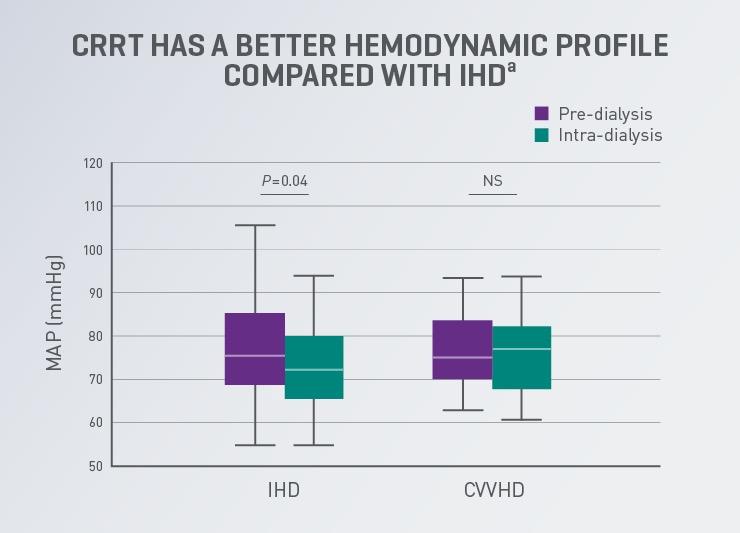
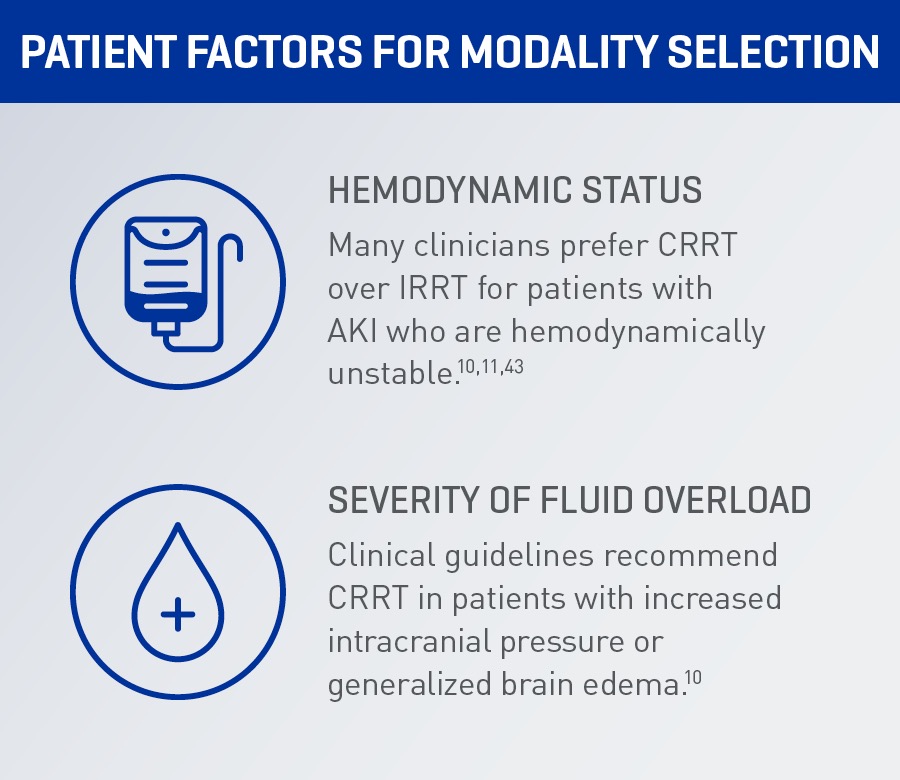
Selection of RRT modality is highly influenced based on the patient’s hemodynamic status and severity of fluid overload. Clinical guidelines recommend using CRRT and Intermittent Renal Replacement Therapy (IRRT) as complementary therapies for patients with severe AKI1, therefore clinicians must decide which modality is appropriate for a particular patient at any one time.
“We suggest using CRRT, rather than standard intermittent RRT, for hemodynamically unstable patients. (Grade 2B)”1
-KDIGO Kidney Disease. Improving Global Outcomes (KDIGO). KDIGO Clinical Practice Guideline for Acute Kidney
CRRT is the preferred RRT modality for patients with AKI who are hemodynamically unstable or require precise fluid management.
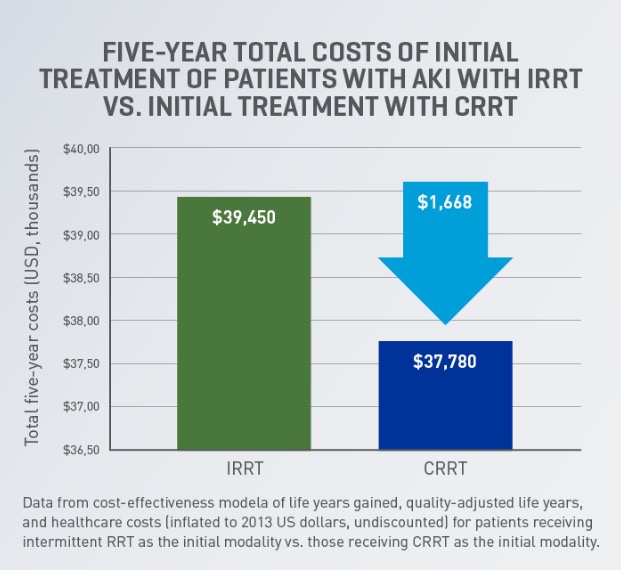
CRRT can be a cost-effective therapy that may provide additional clinical and operational benefits for patients and hospitals
- Initial treatment of patients with AKI using CRRT may be more cost-effective at 5 years post RRT initiation than other RRT modalities.41 A cost-effectiveness analysis found that CRRT may save an estimated US$1,668 over 5 years.41,b,c
- Cost-effectiveness analyses suggest CRRT to be cost-effective compared with intermittent RRT, with dialysis dependence rate as the major driver of cost-effectiveness.42